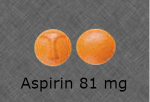
 Highly educated and experienced cardiologists just can’t get it right: the correct dose of aspirin after a heart attack is 81 mg (called low-dose), NOT 325 mg (called high-dose). The current prescribing error rate is 60.9% as published by the American Heart Association in 2014.
Highly educated and experienced cardiologists just can’t get it right: the correct dose of aspirin after a heart attack is 81 mg (called low-dose), NOT 325 mg (called high-dose). The current prescribing error rate is 60.9% as published by the American Heart Association in 2014.
Personal communication with several cardiologists elicits the comment: the higher dose is needed because of the risk of another heart attack — and “in my experience” it just works better. It’s hard to believe this clinical error in this age of quality assurance. The problem is BLEEDING not heart attacks! The stomach BLEEDS due to aspirin and the higher the dose the higher the risk of BLEEDING.
 Just imagine the risk and strain for a recent heart attack victim who vomits blood, needs a transfusion and must undergo a stomach scope — some patients die. From a cardiology standpoint: “they died from something unrelated to the heart attack” — great thinking.
Just imagine the risk and strain for a recent heart attack victim who vomits blood, needs a transfusion and must undergo a stomach scope — some patients die. From a cardiology standpoint: “they died from something unrelated to the heart attack” — great thinking.
Cardiologists completely and totally get it wrong when they simultaneously prescribe high dose aspirin and the anticoagulant warfarin — the ghastly mistake happens 40% of the time.
The chemical reaction of “acetylation” is caused by aspirin within small blood cells called platelets. Acetylation of platelets is responsible for the favorable heart effects of aspirin. It has been known for at least 30 years that 81 mg of aspirin completely acetylates every platelet a person has — more aspirin does no more. According to the 2012 TRITON-TIMI trial:
“We observed no difference between patients taking a high dose versus a low of aspirin as it relates to cardiovascular death, heart attack, stroke or stent thrombosis,” according to Payal Kohli, MD involved in the study and quoted in Science Daily.
Hospital quality improvement programs need the “guts” to just say NO. 325 mg is not correct. Cardiologists are the sweetheart doctors making millions of dollars for hospitals — it should not matter, JUST SAY NO.
It’s almost impossible for even the most proactive patient to question the great doctor that just saved their life. So, hospital quality assurance has an even greater responsibility than usual. The prescribing error needs to be corrected — hospital pharmacists and quality improvement departments need to be strongly involved — this error has gone on far too long.