Posts Tagged UK
Twice the Quality at Half the Price — the NHS in the UK
Posted by qualityhealthcareplease in Hospital Quality, Macro Economics, Restructuring Health Care, UK National Health Service, Variations in Care on May 10, 2013
How do the Brits do it? They made a healthcare system with twice the quality at half the price compared to the US (according to the Commonwealth Fund cost per person per year US $7960 UK $3487, developed country quality rank UK #2 US #7). Simply, they do it by having original ideas and a willingness to adopt good ideas from other countries.
The National Health Service (NHS) of the UK was born in the aftermath of WWII. Taxes pay for the system, which is free to citizens at the point of care. Internally, the system is based on capitation — doctors and hospitals are paid by the size of the population they serve. The system grew to be one of the highest quality and least expensive systems in the world. In the 90’s it was bogged down by waiting lines and old facilities until a modernization push got it back on track around 2000.
The DRG example: In 1983 Medicare adopted a way to pay hospitals with a single payment for each case based on the diagnosis of the patient. This revolutionary idea was called the diagnosis related group or DRG. NHS experts embraced the Medicare cost saving idea and renamed it the HRG (health resource group) and started using it in about 2003. Consequently, by adopting what works, the UK has strikingly transformed the financial workings of the NHS.
The NHS noticed cost variations between providers and solved the problem with “Best Practice Tariffs”. That means if the provider follows a well established guideline they get a full payment, if not, the payment is lower. In the US we call that concept “value based purchasing” (VBP) but the US only has a few pilot projects and only dreams about making VBP happen on a large scale.
The UK decided they wanted better results. The reform was called Payment by Results (PbR) and implemented in 2013. The results they expected were high quality, adequate volume of services, and cost efficiency. The NHS basically tweaked the capitation formula with incentives for the desired results.
The US Affordable Care Act (Obama Care) encourages the aggregation of doctors and hospitals in an economic model called an Accountable Care Organization (ACO). The US thinks it invented the idea behind the “Accountable Care Organization”. Actually, the concept is just a spin-off from the Primary Care Trusts and Hospital Trusts in the UK which have been functioning for over 60 years. Think: “Trust”=”ACO”.
The recent “Perspective” in the New England Journal of Medicine (NEJM 668;16 April 18, 2013, page 1465-1468) describes the recent IOM report requested by Congress. The authors lament the “Geographic Variation in Medicare Services“. The NHS is well known for controlling health care costs. Looking across the pond to the UK, here are some references that might be helpful to them:
- A simple guide to Payment by Results
- A person based formula for allocating commissioning funds to general practices in England: development of a statistical model
- Payment by Results: time for a rethink?
- Regional variation in the productivity of the English National Health Service.
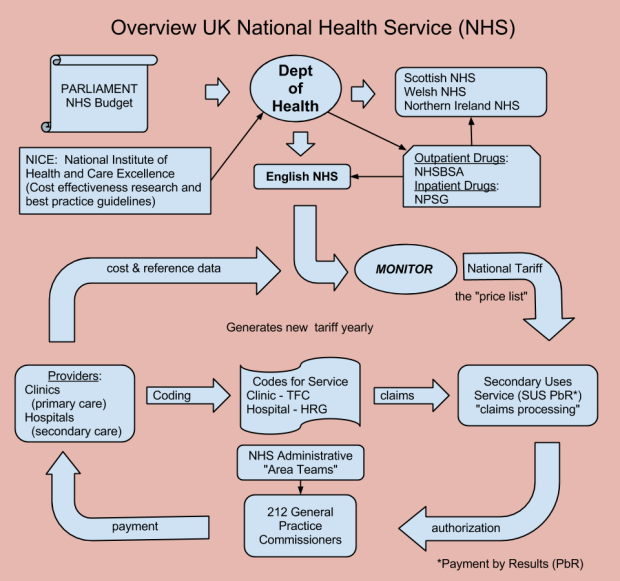
Some understanding about how the NHS works would also be helpful. The following diagram is an overview of how the NHS controls cost associated with hospitals and doctors. They also have a good system for dealing with drugs and devices — a good topic for a future blog.
(figure revised 7/11/13)
Other charts of organization can be found at Nuffield Trust – New Structure of the NHS slideshow, NHS website – new structure, and History of the NHS.
In the UK 90% of health care is controlled by the government and 10% by the private sector. The UK Parliament sets a budget for health care which is administered by the Department of Health. Based on the funds allocated in the budget the Department of Health makes a national price list for services (unlike the US where there is no cap on expenditure) .
The “SUS” approves payments to providers based on the national price list (national tariff) and adds the features of PbR (payment by results). The commissioners are the paymasters and transfer funds to the providers. The providers keep track of actual costs and must provide cost data to the Department of Health (unlike the US where real costs are proprietary information and hospitals use the infamous “chargemaster“).
The US could learn a lot from other countries. The NHS in the UK seems very willing to share what they have learned over the years — and it is in English. The old saying “America and England are two countries separated by a common language” is especially true for health care.